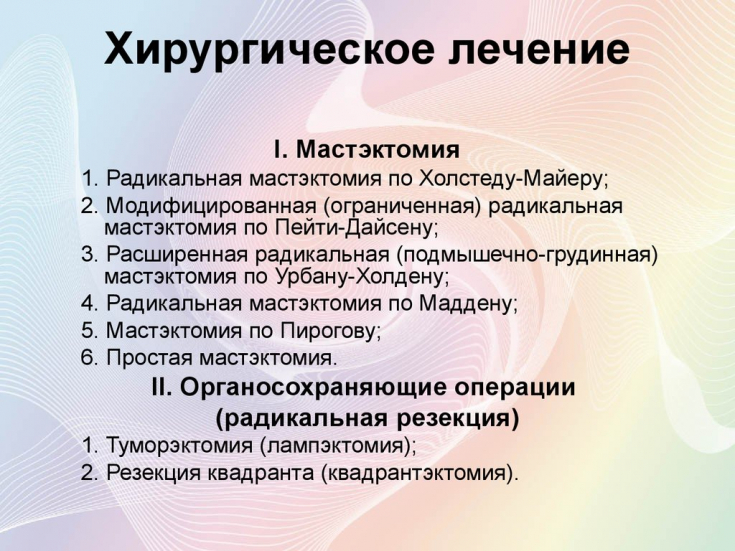
Surgical treatment of patients with breast cancer (BC) remains the main method in the complex therapy, as indicated in all modern standards, recommendations and protocols.
The leading methods of surgical treatment for breast cancer are mastectomy (ME), organ-preserving surgery (CCA), simultaneous reconstructive and oncoplastic intervention. The number of mastectomies continues to be significant − 40-60% despite improvements in early detection and increased use of CCA.
One of the most significant complications after mastectomy is post-mastectomy syndrome, accompanied by severe pain, which significantly impairs the quality of life of patients after removal of the mammary gland. Find out in the article on estet-portal.com about the main methods of preventing mastectomy complications.
Complications after mastectomy
In recent years, the number of mastectomies has slightly increased due to greater attention to the detection of multicentric growth of breast cancer, the spread of the use of magnetic resonance mammography (MRM) in the diagnosis and the detection of an oncological process by other methods (ultrasound diagnostics, mammography).
Follow us on Instagram!
The most common complication after mastectomy is post-mastectomy syndrome. This is a complication that includes lymphostasis of the upper limb, contractures of the shoulder joint, paresthesia and numbness of the skin of the inner surface of the shoulder, chronic pain syndrome of the shoulder and chest wall on the side of the operation.
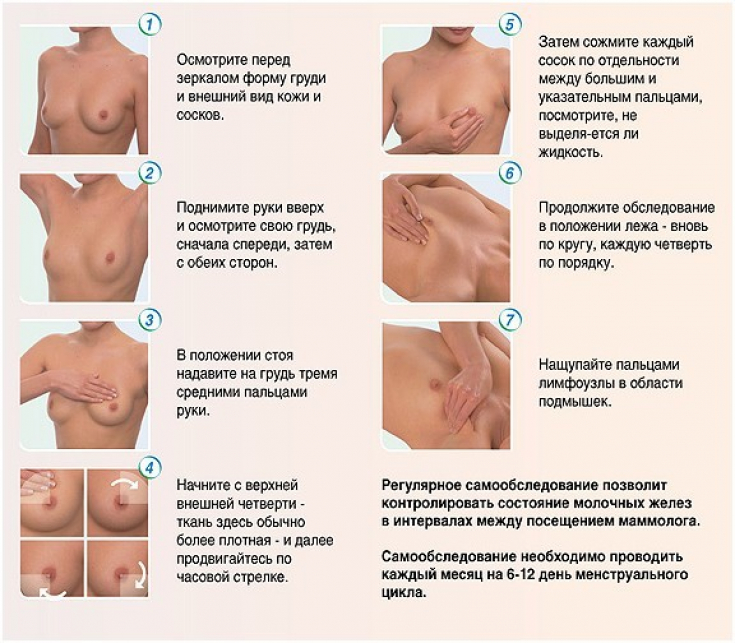
Characteristics of methods for diagnosing breast neoplasms
Recently, this syndrome occurs less frequently compared to the period when, for breast cancer, operations were performed as a mastectomy according to the Halsted or Pati method (70-90s of the XX century). Now they mainly carry out a modified mastectomy according to Maden, after which the frequency of the above complications is minimized, but not all.
For example, the incidence of lymphostasis and contractures is reduced to 10-20%, but the frequency of paresthesia and pain remains at the level of 50-70%.
Therefore, in recent literature, this syndrome refers mainly to chronic pain that lasts more than 3 months after mastectomy. The presence of pain up to 3 months after surgery is considered quite possible as a result of surgical trauma. Chronic postoperative pain syndrome (CPPS) occurs in 52% of cases not only after mastectomy, but also after organ-preserving operations (quadrantectomy, tumorectomy, radical sectoral resections).
Causes of pain after mastectomy
The main cause of complications after mastectomy may be damage to the neurovascular bundles that pass in the armpit. These include the subclavian artery and vein with elements of the brachial plexus, the subscapular artery, vein and nerve, the lateral thoracic artery, vein and long thoracic nerve, and the intercostal-brachial cutaneous nerves.
Preoperative diagnosis of breast neoplasms
These main neurovascular structures are freed from fascia, cellular tissue and lymph nodes during lymph node dissection. During this procedure, part of the nerve fibers may be injured.
This is especially characteristic of the intercostal-brachial cutaneous nerves, as they pass from the chest wall to the shoulder in a horizontal direction.
Recent studies on the development of complications of mastectomy found that the frequency of their occurrence was higher in cases where lymph node dissection was more traumatic, and more lymph nodes were removed, and not always affected by metastases.
The study of the causes of pain syndrome after mastectomy also showed that it is always present and more pronounced in those cases where there were its initial manifestations before the operation. Separate studies have shown that the cause of chronic pain after mastectomy is damage to the intercostal-brachial nerves during axillary lymph node dissection.
Practical anatomy of the ligamentous apparatus of the breast: fighting myths
Preventive measures for complications after mastectomy
To prevent the development of these complications in recent decades, it is recommended to remove the axillary lymph nodes less traumatically, to preserve the subscapular vein and its branches as much as possible, to preserve the branches of the lateral thoracic vein and sensory nerve fibers − intercostal-brachial branches.

Axillary lymphadenectomy techniques are known that involve preservation of the intercostal-brachial nerves. This prevents the development of contractures of the shoulder joint and impaired skin sensitivity of the upper limb and chest wall during mastectomy.
These techniques are characterized by a satisfactory aesthetic effect and satisfactory rehabilitation of patients in the postoperative period. To prevent traumatic lymphadenectomy, in the absence of metastases in the lymph nodes, it is advisable to carry out only isolated removal of borderline lymph nodes with mandatory histological examination.
Dangerous breast implants: the main risks of mammoplasty
In such cases, the vessels and nerves are not damaged at all and the complications described above do not occur. But in the case when there are metastases in the axillary lymph nodes, they should be removed as completely as possible in one block with the surrounding tissue, blood vessels and nerves.
The next step in the prevention of mastectomy complications in breast cancer is combined anesthesia − combination of general anesthesia with local anesthesia. To do this, before opening the skin, infiltration anesthesia is performed with a local anesthetic (0.5% lidocaine, procaine, bupivacaine).
Also, in order to reduce postoperative disability, restore the quality of life of patients after surgical treatment for breast cancer, it is proposed to conduct psychological rehabilitation before surgery.
Do breast implants cause autoimmune diseases







Add a comment