Parry-Romberg syndrome (also known as progressive facial hemiatrophy) is a rare disorder characterized by progressive degeneration of tissues under the skin, usually on only one side of the face (facial hemiatrophy), but sometimes spreading to other parts body.
An autoimmune mechanism is suspected, and the syndrome may be a variant of localized scleroderma, but the exact cause and pathogenesis of this acquired disorder remain unknown. Possible consequences of sympathectomy have been reported in the literature. The syndrome has a higher prevalence among women and usually appears between the ages of 5 and 15.
In addition to the connective tissue disorder, the condition is sometimes accompanied by neurological, ocular, and oral symptoms. The range and severity of the associated symptoms and findings vary greatly.
In the estet-portal.com article, you can detail the etiology, pathogenesis, and current guidelines for the diagnosis and management of Parry-Romberg syndrome.
Clinical characteristics of progressive facial hemiatrophy

The disease progressively spreads from the zygomatic bone region, resulting in atrophy of the skin and its appendages, as well as underlying subcutaneous structures such as connective tissue (fat, fascia, cartilage, bone) and/or muscles on one side of the face. The mouth and nose usually deviate towards the affected side of the face.
The process may eventually spread to tissues between the nose and upper lip angle, upper jaw, corner of the mouth, eye and brow area, ear and/or neck.
The syndrome may also begin as a localized area of scleroderma in the frontal region, manifested by hair loss and a linear scar extending down the middle of the face on the affected side.
Often resembles a saber wound scar and is indistinguishable from the scar seen in frontal linear scleroderma.
Features of the course of the main forms of scleroderma
In 20% of cases, the hair and skin covering the affected areas may become hyperpigmented or hypopigmented. In 20% of cases, the disease can spread to the ipsilateral (on one side) or contralateral (on the opposite side) side of the neck, trunk, arm or leg.
The disease has been reported to affect both sides of the face in 5-10% of cases.
The disease may progress for several years before eventually going into remission.
Follow us on Facebook
Neurological disorders of Parry-Romberg syndrome
Neurological disorders are common. Approximately 45% of people with Parry-Romberg syndrome also have trigeminal neuralgia and/or migraines.
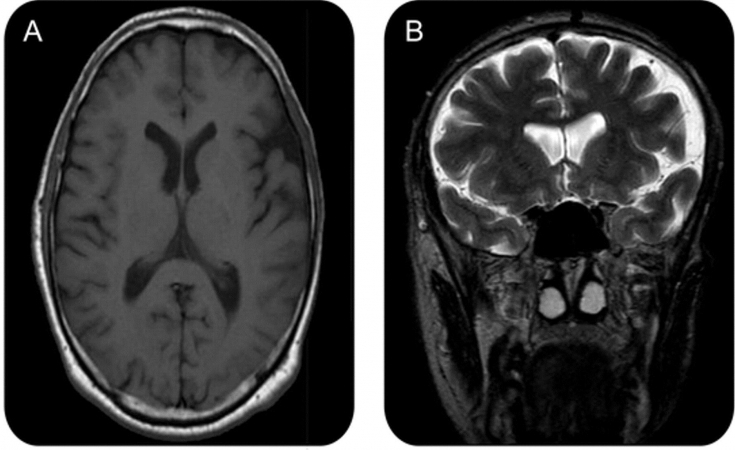
10% of those affected develop a seizure disorder as part of the disease. Epileptic seizures, as a rule, are Jacksonian in nature (characterized by contraction of the muscle group, which subsequently spread to neighboring muscles) and occur on the side opposite the affected side of the face. Half of these cases are associated with abnormalities in both the gray and white matter of the brain — usually ipsilateral, but sometimes contralateral — which are detected during magnetic resonance imaging (MRI) scans.
Enophthalmos (inward displacement of the eyeball) is the most common ocular pathology seen in Parry-Romberg syndrome, which is caused by a decrease in subcutaneous tissue around the orbit. Other manifestations include ptosis, pupillary constriction (miosis), reddening of the conjunctiva, and decreased sweating (anhidrosis) of the affected side of the face.
Collectively, these signs (ptosis, miosis, enophthalmos) are called the Claude Bernard-Horner syndrome.
Other visual impairments include ophthalmoplegia (paralysis of one or more extraocular muscles), strabismus, uveitis, and iris heterochromia.
Dental manifestations of Parry-Romberg syndrome
Oral tissues, including the tongue, gums, teeth, and soft palate, are commonly involved in the pathological process in Parry-Romberg syndrome:
• 50% of people develop dental anomalies such as delayed eruption, root resorption on the affected side;
•
• 25% develop atrophy of one side of the upper lip and tongue.
Watch the most interesting videos on our channel in Youtube
What is the cause of progressive hemiatrophy of the face
The fact that some people affected by this disease have circulating antinuclear antibodies in their serum supports the theory that Parry-Romberg syndrome may be an autoimmune disease, specifically a variant of localized scleroderma.

Several cases have been reported where more than one family member was affected, leading to the suggestion of an autosomal dominant inheritance pattern. However, there has also been at least one report of pathology in one of the monozygotic twins, casting doubt on this theory.
The National Organization for Rare Diseases has stated that there is no evidence that Parry-Romberg syndrome can be passed on to children.
Various other theories about cause and pathogenesis have been proposed, including changes in the peripheral sympathetic nervous system (possibly resulting from trauma or infection involving the cervical plexus or sympathetic trunk).
Diagnosis of progressive hemiatrophy of the face
Diagnosis can be made solely on the basis of the history and physical examination of people who have only facial asymmetry. For those reporting neurological symptoms such as migraine or seizures, brain MRI is the imaging modality of choice. Diagnostic lumbar puncture and serum autoantibody testing may also be indicated. Oligoclonal bands and an elevated IgG index can be detected in 50% of patients.
Vulvar lichen sclerosus: diagnosis and treatment
Modern opportunities for the management of Parry-Romberg syndrome
Medical management may include immunosuppressants such as methotrexate, corticosteroids, cyclophosphamide, and azathioprine.

Affected individuals may benefit from autologous fat grafting to restore a more normal facial contour. However, large volume defects may require microsurgical reconstructive surgery, which may involve transfer of an insular paravascular fasciocuticular flap or free flap from the groin, rectus abdominis muscle (the transverse rectus abdominis or "TRAM" flap), or the latissimus dorsi muscle to face.
Thank you for staying with estet-portal.com. Read other interesting articles in the "Dermatology" section. You may be interested in What can cause systemic scleroderma









Add a comment