Eyelid surgery – this is one of the most frequently performed surgical interventions in aesthetic surgery. Patients want to eliminate age-related changes that primarily appear on the delicate skin of the eyelids. But any surgical intervention – this is a risk that can always lead to the development of complications. Dry eye syndrome is one of the most common complications after blepharoplasty. The name of the syndrome speaks for itself: after surgery, the patient may have a disruption in the secretion of tears, which is necessary for a very important physiological process – moisturizing the eyeball.
Methods of diagnosis and treatment of dry eye syndrome
Dry eye syndrome in ophthalmology it is commonly called dry keratoconjunctivitis. This disease can develop as a complication after manipulations in the eye area, as well as an independent pathology. The etiological factors of dry keratoconjunctivitis can be prolonged use of drugs that regulate intraocular pressure, prolonged work at the computer, innervation disorders as a result of trigeminal nerve paresis, and other causes. Predominantly women over the age of 40 are susceptible to the disease. Manifested syndrome "dry eye" decrease and even complete cessation of the secretion of tears, as well as atrophy of the lacrimal glands.
Dry Eye Syndrome:
- clinical picture of dry eye syndrome;
- methods for diagnosing dry eye syndrome;
- methods of treatment of dry eye syndrome.
Clinical presentation of dry eye syndrome
In the clinical picture of the "dry eye" syndrome; There are 4 stages of the disease:
- chronic blepharoconjunctivitis – at this stage, the patient complains of pain, itching and burning in the eyes, sensation of a foreign body and the presence of mucous discharge. On examination, there is loosening of the conjunctiva, redness and thickening of the edges of the eyelids, accumulations of mucous discharge in the lower fornix;
- epithelial corneal dystrophy – at this stage, patients develop photophobia, a feeling of dry eyes, and there are no tears when laughing, crying, and various eye irritations. On the surface of the cornea, a large number of movable threads are observed, which are attached to the cornea at one end, and the second – hanging freely;
- filamentous keratitis – at this stage, there are complaints of a sharp deterioration in vision, a sensation of a foreign body and pain in the eye. On examination, a large number of mucous filaments are observed, which in their structure are tubules of epithelial cells filled with mucus;
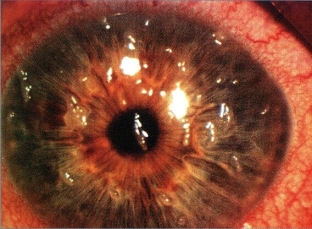
- deep corneal xerosis is manifested by a complete lack of vision. The conjunctiva of the eyeball in such patients is dull, grayish in color, superficial corneal vascularization occurs. In especially severe cases, the addition of uveitis and iridocyclitis is possible.
Methods for diagnosing dry eye syndrome
If a patient who has undergone blepharoplasty or other aesthetic surgery in the eye area develops signs of "dry eye" syndrome; He definitely needs to consult an ophthalmologist. Diagnostic process of "dry eye" syndrome begins with a detailed history taking and a standard examination of the organ of vision with targeted biomicroscopy of the edges of the eyelids, conjunctiva and cornea. Additional research methods are:
- sighted biomicroscopy of the anterior eyeball;
- testing tear production and tear film stability;
- conducting special diagnostic tests necessary to clarify the changes associated with the dry eye syndrome.
Methods of treating dry eye syndrome
Treatment of dry eye syndrome is symptomatic. Such patients are prescribed gel or water-based drugs that are tear substitutes:
- hydroxypropyl methylcellulose with dextran;
- carbomer;
- hyaluronic acid sodium salt;
- polyacrylic acid with sorbitol, etc.
If artificial tears do not achieve the desired effect – lacrimal duct obturators are used. Additionally, patients with dry eye syndrome Antibacterial and anti-inflammatory drugs are recommended, the appointment of which is necessary to prevent the addition of a secondary infection. In especially severe cases, surgical treatment is necessary, which consists in applying a special biocoating to the surface of the eyeball.







Add a comment