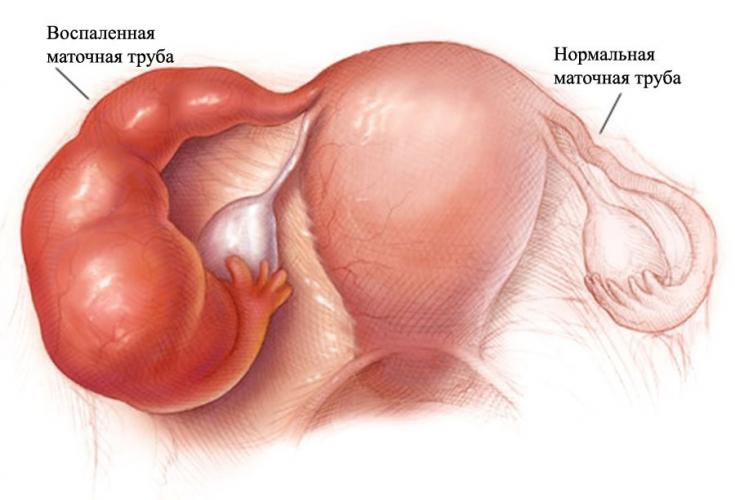
Salpingitis is an inflammation of the fallopian tube, most commonly caused by an infection. This disease can have dire consequences for a woman's body, starting with infertility and ending with diffuse peritonitis.
It was believed that the causative agents of salpingitis are usually chlamydia or gonococci, however, studies have shown that opportunistic microflora most often becomes the cause of the disease.
On estet-portal.com read about the main features of the diagnosis and treatment protocols for salpingitis.
Etiology of salpingitis: main pathogens
Neisseria gonorrhoeae and Chlamydia trachomatis were originally thought to be the only pathogens causing acute salpingitis.
Polymicrobial flora have been found to be the most common cause of salpingitis.
Pathogens are associations of microorganisms that commonly colonize the lower genital tract, such as Gardnerella vaginalis, Escherichia coli, Haemophilus influenzae, group B beta-hemolytic streptococci, non-hemolytic streptococci, Mycoplasma hominis, etc.
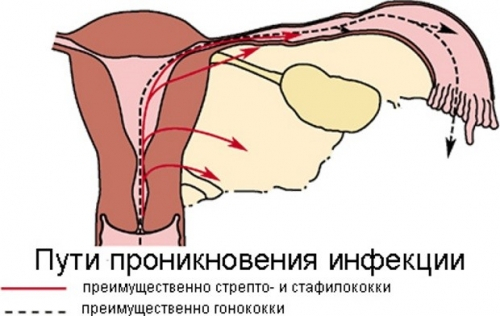
Salpingitis is believed to be an ascending infection resulting from the direct spread of microorganisms from the endocervix to the endometrium and then the fallopian tube mucosa.
You may also be interested in: Effective treatment of oophoritis or how to beat inflammation
Factors contributing to the development of salpingitis
There are several factors that can contribute to the spread of infection from the lower genital tract, and, as a result, the development of salpingitis.
Among them, the main ones are:
• use of instruments for setting up an intrauterine device;
• carrying out curettage of the uterus;
• endometrial biopsy;
• hormonal changes during menstruation causing changes in the cervix leading to the disappearance of the mechanical barrier, including bacteriostatic cervical mucus.
The spread of infection can also occur with lymph flow or hematogenously.
Read the latest articles in Telegram!
Clinical picture of salpingitis
The clinical picture of salpingitis is very diverse. The lesion can either be asymptomatic or be accompanied by an intense pain syndrome, for example, with the development of diffuse peritonitis.
Most often observed with salpingitis:
• pain in the lower abdomen;
• pain on palpation of the cervix;
• painfulness of the appendages;
• Temperature above 38.3 ° C;
• abnormal mucopurulent discharge from the cervix or vagina;
• irregular bleeding;
• dysuric phenomena;
• vomiting;
• proctitis symptoms;
• elevated levels of ESR and/or C-reactive protein.
It is not always easy to suspect salpingitis, however, this disease must always be kept in mind, making a differential diagnosis with other diseases and conditions accompanied by similar symptoms.
Pelvioperitonitis and parametritis – formidable complications in gynecology
Basic treatment regimens for salpingitis
Empirical treatment of salpingitis should be initiated in patients at risk of genital infections if they complain of pelvic pain and if one or more of the following minimum criteria are met: tenderness and/or tenderness of the uterus, adnexa, or cervix.
The main drugs for the treatment of salpingitis – these are 3rd generation cephalosporins (ceftriaxone, cefoxitin) in combination with tetracyclines (doxacycline).
Regulation #1:
Ceftriaxone 250 mg IM once, plus doxycycline 100 mg twice daily for 14 days, with metronidazole 500 mg twice daily for 14 days .
Regulation #2:
Cefoxitin 2 g IM single dose plus probenecid 1 g IM single dose plus doxycycline 100 mg twice daily for 14 days with metronidazole 500 mg twice a day for 14 days.
Typically, antibiotic therapy for salpingitis is prescribed for two weeks. The addition of metronidazole or clindamycin is recommended for better anaerobic coverage.
Latent sexual infections: an invisible danger






Add a comment