One of the five most common causes of maternal death is postpartum hemorrhage (Postpartum Hemorrhage − PPH) − an emergency in obstetric practice that can be foreseen and quickly removed.
Promptly treating this complication can significantly reduce maternal mortality.
Check out the article on estet-portal.com for the latest clinical guidelines for managing patients with postpartum bleeding.
- The concept of early postpartum hemorrhage
- Diagnostic criteria for postpartum haemorrhage
- Stages of postpartum haemorrhage
- Medicated treatment of postpartum haemorrhagei
The concept of early postpartum haemorrhage
Early or primary postpartum haemorrhage occurs within the first 24 hours after delivery; delayed or secondary − 24 hours to 12 weeks postpartum.
According to the traditional definition, postpartum haemorrhage − is blood loss 500 ml after vaginal delivery or ≥1000 ml after caesarean section.
Follow us on Instagram!
The American College of Obstetricians and Gynecologists revised the definition in 2017 and found that postpartum haemorrhage − cumulative blood loss > 1000 ml or bleeding associated with signs and symptoms of hypovolemia within 24 hours postpartum (vaginal or caesarean section).
Patients with a cumulative loss of 500-999 ml of blood require enhanced surveillance and interventionand according to clinical indications.
Diagnostic criteria for postpartum haemorrhage
will help determine the etiology of early postpartum hemorrhage.
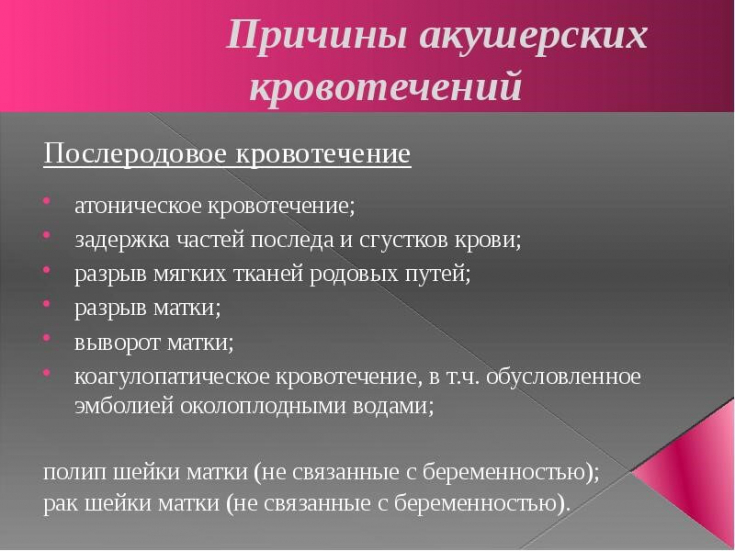
1. Tone:uterine atony (ineffective uterine contraction after delivery of the placenta) − main cause of bleeding, which may mask profuse bleeding. This may produce a large number of clots that must be removed.
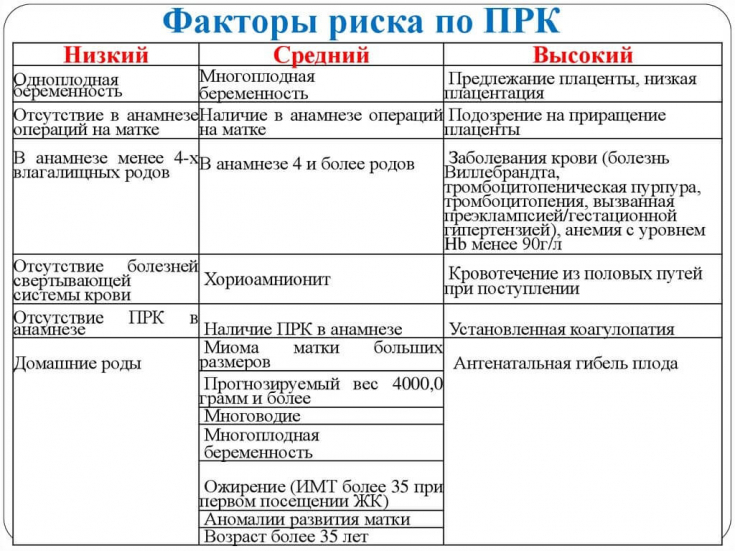
Pathology of placental attachment: placenta previa, placenta accreta and placental abruption also cause bleeding because they reduce the effectiveness of uterine contraction and create conditions for postpartum hemorrhage.
2. Tissue:Tissue debris, placenta, retained membranes and blood clots, or an extra lobe of the placenta can cause bleeding because it prevents the uterus from contracting normally.
3. Trauma:for vaginal delivery, ruptures of the vagina, cervix, and uterus should be considered; at caesarean section − consider occult bleeding from damaged uterine arteries that have contracted, and as a result of this, a retroperitoneal hematoma could form; bleeding from the hysterotomy site.
Ultrasoundwill help identify bleeding.
4. Thrombin:coagulopathy, DIC may be due to congenital or acquired hemorrhagic diathesis or a decrease in the level of blood clotting factors during massive bleeding.
Acute coagulopathymay result from:
placental abruption;Dangerous conditions: dropsy of pregnancy Stages of postpartum haemorrhage
help assess the severity of bleeding and determine the next course of action:
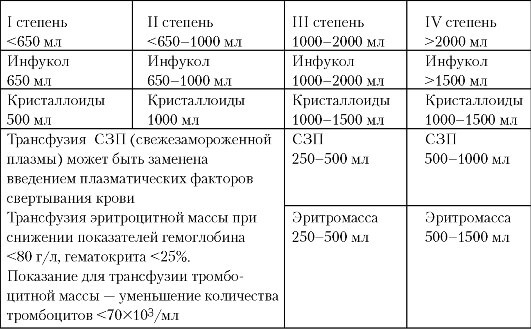
1st stage− normal vital signs and laboratory values: blood loss ≥1000 ml during labor;
2nd stage− normal vital signs and laboratory values: continued bleeding up to 1500 ml or the patient needs more than 2 uterotonics;
3rd stage− violation of the main indicators of the state of the body and laboratory values:
oliguria;- bleeding that continues when assessing blood loss> 1500 ml;
- ≥2 RBCs have been transfused;
- patient at risk of occult bleeding (after caesarean section) and DIC.
− the development of cardiovascular collapse, which is associated with massive bleeding, severeth hypovolemic shock or amniotic fluid embolism.
1.
Oxytocin−10-40 UNITS add to 500-1000 ml saline or lactate Ringer's solution, inject slowly. 2.
Methylergometrine− 0.2 mg IM or myometrium every 2-4 hours. 3.
15-methyl PGF2 alpha− 0.25 mg IM or myometrium every 15 minutes (up to 8 doses). 4.
Misoprostol− 600-1000 micrograms orally, sublingually or per rectum, 1 dose. 5.
Tranexamic acid− 1 g over 10 minutes (add 1 g to vial in 100 ml saline) every 30 minutes until bleeding is controlled.
What you need to know about your first IVF procedure It is important not only to timely diagnose a rapid decrease in the level of erythrocytes, but also to recognize coagulopathy in a timely manner.
During treatment in case of bleeding, it is important:
control blood loss;
- limit thrombocytopenia;
- prevent consumption coagulopathy;
- maintain systolic blood pressure at least 80-100 mmHg. Art.
.
Consequences of pyelonephritis during pregnancy Postpartum haemorrhage can be prevented by continuous monitoring of maternal parameters and accurate assessment of blood loss during and after delivery.
Treatment provided in time, depending on the situation, will significantlyreduce maternal mortality
.







Add a comment