Miscarriage occurs in one in five pregnant women and is one of the most common complications of pregnancy.
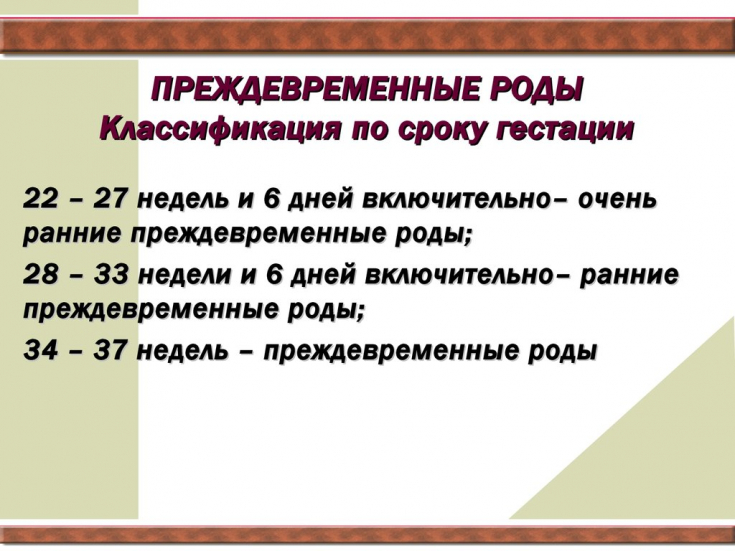
Premature birth, which occurs in approximately 7% of women giving birth, is the largest cause of neonatal complications and death. Both miscarriage and preterm birth significantly affect the physical and psychological well-being of expectant parents and have serious consequences for them.
Find out in the article on estet-portal.com whether there are risks of premature birth due to thyroid pathology.
- The influence of thyroid diseases on the development of preterm birth
- Premature birth and ATPO indicators
- The advisability of hormonal therapy for the risk of developing premature birth
The influence of thyroid diseases on the development of preterm birth
The study by American scientist Alex Stagnaro-Green was the first to demonstrate a link between elevated levels of thyroid peroxidase antibodies (TPO) and an increased incidence of preterm birth.
Follow us on Instagram !
The aim of the study was to evaluate the incidence and causes of postpartum thyroiditis. Combining data from 552 women, the researcher found that high thyroid ATPO levels are a marker for pregnancies that may be considered at risk compared to pregnant women without elevated levels. ATPO indicators.
Premature birth and ATPO indicators
A few years later, Belgian scientists conducted a study to evaluate whether there was an increased risk of developing subclinical hypothyroidism (SH) during pregnancy in women with autoimmune thyroiditis (AIT), and to examine whether mild thyroid dysfunction could lead to undesirable consequences. in obstetrics, in particular, premature birth.
Thanks to the study, it was reported that preterm birth is more common in women with high levels of AIT compared to pregnant women without AIT.
Small randomized controlled trials and several meta-analyses have confirmed that AIT and FH are strongly associated with the risk of miscarriage and preterm birth, and have suggested that treatment with levothyroxine may reduce these risks.
Risk factors and modern methods of preventing the development of postpartum depression
A decisive answer to this controversial question was recently obtained in the double-blind, placebo-controlled TABLET study (Thyroid AntiBodies and LEvoThyroxine study), which was conducted by British scientists to investigate whether treatment with levothyroxine would increase live birth rates after 34 years of age. weeks of pregnancy in women with euthyroidism and AIT who have a history of miscarriages or infertility. Or preterm birth is more common in pregnant women with AIT compared to pregnant women without diseases thyroid gland?
The feasibility of hormonal therapy for the risk of premature birth
Women from 49 UK hospitals took part in the study. All women were aged between 16 and 40 years with a history of preterm birth or infertility within 12 months. Screening included blood tests for ATPO, thyroid-stimulating hormone (TSH) and free thyroxine (T4). Participants were assigned to take 1 tablet (50 mcg) of levothyroxine or placebo daily before conception. During pregnancy, women had three visits to the doctor: at 6-8 weeks, 16-18 weeks and 28 weeks. A total of 476 women were assigned to treatment with levothyroxine and 476 to placebo.
Vegetarianism during pregnancy: recommendations from experts in the field of nutrition
56.6% in the levothyroxine-treated group and 58.3% in the placebo group became pregnant, and birth rates were similar in the two groups (37.4 and 37.9%). There were also no differences in the incidence of preterm birth, miscarriages and other adverse effects in mothers and newborns in both groups. Thus, the use of levothyroxine in women with elevated TPO levels and euthyroidism was NOT associated with higher rates of live birth than placebo.
Thus, the British study rejected the recommended benefits of treatment with hormone replacement therapy in pregnant women with chronic AIT and euthyroidism. These results confirmed the findings of another recent Chinese study, which involved 600 women who had undergone in vitro fertilization and half of whom were taking levothyroxine. According to the results of the study, scientists did not find any benefits or better results in women receiving hormone replacement therapy.
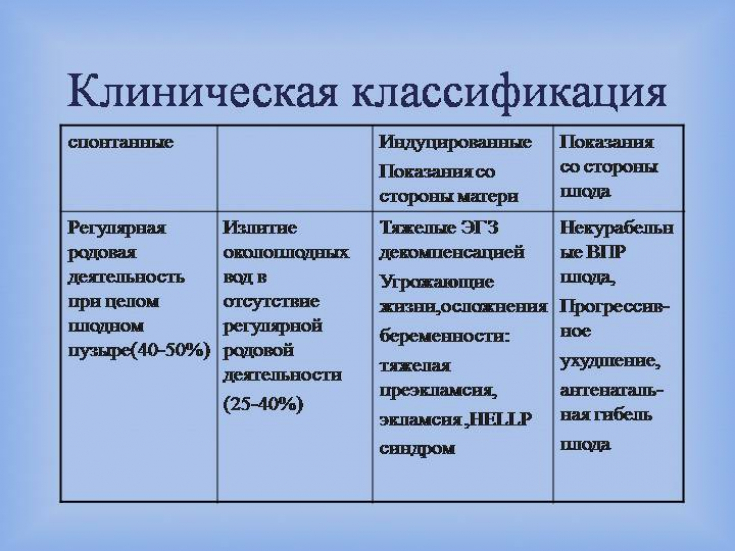
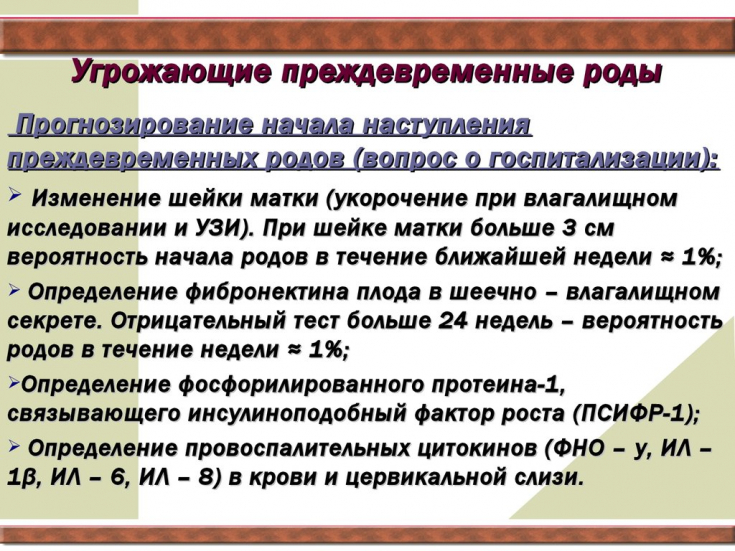
Modern approaches to the prevention of preterm birth
The American Thyroid Association guidelines state that there is insufficient evidence to definitively determine whether levothyroxine therapy reduces the risk of pregnancy loss and preterm birth.
However, since one study has shown that women with AIT are prone to developing hypothyroidism during pregnancy and elevated TSH concentrations can lead to pregnancy loss, it is advisable to monitor and treat these patients if the TSH level exceeds 4.0 mmol/L.
Research results indicate that treating women with AIT with levothyroxine before pregnancy does not increase fertility and does not affect the intelligence of children in the future. This finding supports a conservative approach when targeting women of childbearing age early in pregnancy.
Urinary tract infections during pregnancy: evidence-based medicine







Add a comment