Gestational diabetes mellitus (GDM) − is diabetes mellitus of any etiology or impaired glucose tolerance (IGT) that first appeared or was diagnosed during pregnancy.
Many factors contribute to the onset of gestational diabetes, including ethnicity, age, and family history. However, obesity is an independent risk factor for the development of GDM, with an incidence 2-3 times higher in obese and overweight women than in normal weight women.
Find out in the article on estet-portal.com what threatens gestational diabetes and what are the causes of its occurrence.
- The impact of gestational diabetes on fetal development
- Long-term risks in women with gestational diabetes
- Hormonal changes as predictors of gestational diabeteseta
Impact of gestational diabetes mellitus on fetal development
Obesity and insulin resistance affect placental function, resulting in an increased supply of glucose, free fatty acids and amino acids to the fetus. Maternal hyperglycemia causes fetal hyperglycemia and, as a consequence, fetal pancreatic hypertrophy/hyperplasia and hyperinsulinemia .
Follow us on Instagram!
Insulin has a direct effect on fetal cell division, which leads to macrosomia, which is one of the main consequences of hyperglycemia during pregnancy. The risks of difficult labor and maternal/neonatal complications and associated fetopathies have been confirmed in large cohortsof studies.
Long-term risks in women with gestational diabetes
Long-term risks associated with fetal macrosomia in women with GDM contribute to childhood overweight and metabolic changes that may increase the risk of cardiovascular disease .
Normal-weight women with GDM who carefully monitor blood glucose levels have no higher incidence of macrosomia in newborns than women without a history of diabetes mellitus.
Causes and mechanisms of abdominal pregnancy
At the same time, obese women with normal glucose tolerance are twice as likely to have children with macrosomia. Considering that the prevalence of obesity is approximately ten times higher than that of GDM, it is clear that the lifestyleof the mother has a huge impact on the development of this pathology.
Hormonal changes as predictors of gestational diabetes
In recent years, leptin has been shown to play an important role in the development of GDM. A significant number of studies have found an increase in leptin levels in GDM. In addition, hyperleptinemia in early pregnancy predicts an increased risk of developing GDM in late pregnancy and is independent of maternal obesity.
A study was conducted on 823 women from the 13th week of pregnancy to delivery. Women with leptin levels greater than 31.0 ng/mL are 5 times more likely to develop GDM compared with women with leptin levels <14.3 ng/mL.
In addition, a strong linear correlation between an increase in maternal plasma leptin and an increase in the risk of developing GDM can be observed for every 10 ng / ml increase in leptin concentration, which will be associated with a 20% increase in the risk of GDM. The level of leptin in the amniotic fluid at 15-17 weeks of gestation is directly related to the amniotic insulin concentration.
Strategies for managing pregnancy in multiple sclerosis
such as tumor necrosis factor (TNF) and IL6. TNF is one of the molecules that is responsible for the development of insulin resistance. Comparison of placental gene expression in normal and complicated GDM pregnancies has shown that increased leptin synthesis in GDM is associated with higher production of pro-inflammatory cytokines, such as IL6 and FNS, which causes chronic inflammation.
So, compared with women with normal pregnancy, the placental expression of leptin in patients with GDM is increased. On the other hand, leptin independently increases the production of TNF and IL6 by monocytes and stimulates the production of chemokines.
Thus, a vicious circle of inflammatory processes develops. Hyperinsulinemia in GDM may further stimulate leptin production. Elevated levels of leptin, in turn, increase inflammation.
Medicated treatment of postpartum haemorrhage For
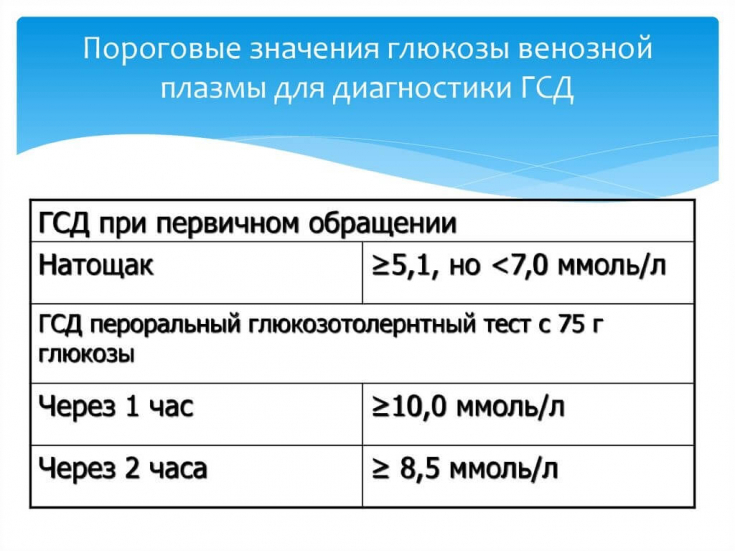
diagnosis of gestational diabetes mellitus, WHO criteriaare used, according to which the diagnosis is made at a glucose level:
on an empty stomach in venous blood plasma ≥ 7 mmol/l;- 2 hours after taking 75 g of glucose (glucose tolerance test) - ≥ 7.8 mmol/l;
- for random glucose determination - ≥ 11.1 mmol/l.
- Screening for GDM is done at 16-18 weeks of gestation. A significant number of prospective studies support the use of the 75 g glucose tolerance test during pregnancy.






