are extremely common among women of reproductive age. At the same time, in half of the cases, the risk of recurrence of the disease within 6-12 months and the development of mixed flora remains, and 20% of patients are prone to recurrent diseases. Due to the prevalence of bacterial vaginosis and possible relapses, the treatment of this pathology requires special attention from the doctor.
Read on estet-portal.com the European guidelines
on the diagnosis and treatment of bacterial vaginosis.Clinical presentation of bacterial vaginosis
Microorganisms that most often cause inflammatory diseases of the vagina associated with pathogenic bacteria, as well as Trichomonas and fungi.
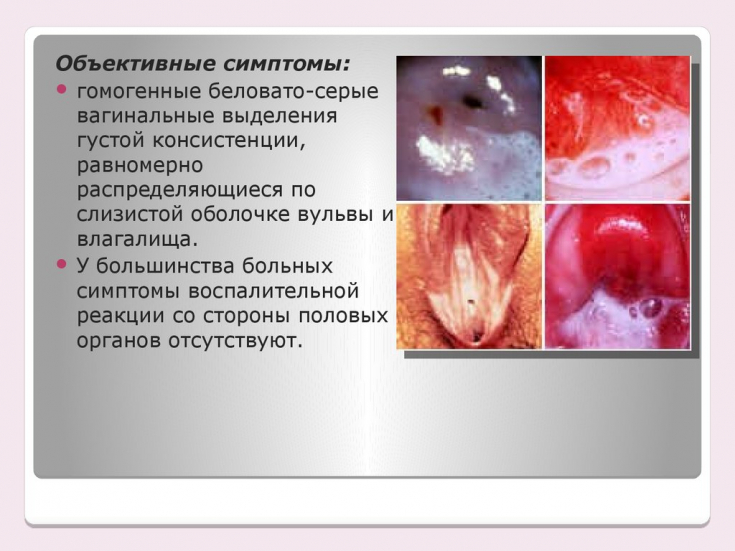
Follow us onInstagram! The clinical picture of bacterial vaginosis of the disease has a rather vague symptomatology, accompanied by such complaints and manifestations as vaginal itching, allergic manifestations or dermatitis of the external genital organs.
Complications after cervical radiotherapy Bacteriological examination may show plating of chlamydia and gonococci in vaginal discharge. But in a third of women with abnormal vaginal discharge, in addition to an unpleasant odor, other complaints may not be observed.
This greatly complicates the provision of timely assistance, since the asymptomatic course of bacterial vaginosis does not contribute to the timely application for specialized care.
Problems of timely treatment of vaginitis
Many women, in the presence of symptoms from the genitourinary system, do not immediately seek help, but start therapy on their own, which is not always effective and can lead to resistance of the bacterial flora to the antibiotic therapy of vaginitis.
What is the danger of migraine during pregnancy The main types of bacterial vaginosis
Bacterial vaginosis − the most common cause of abnormal vaginal discharge in women of reproductive age. Its development is usually associated with vaginal dysbiosis, which causes the appearance of mainly anaerobic microorganisms (Gardnerella vaginalis, Prevotella, Atopobium vaginae, Mycoplasma hominis, Mobiluncus), which cause inhibition of the development of lactobacilli and changes in the pH of the vagina.

Preoperative diagnosis of breast neoplasms In more than 60% of healthy women during pregnancy and the premenopausal period, there is a high tendency to develop candidal vaginitis, which subsequently creates a favorable background for the development of the pathological process. Minimal candidal seeding is found in girls in the prepubertal period and in women in the postmenopausal period who use hormone replacement therapy. At the same time, 75% of women have the risk of experiencing candidal vaginosis at least once in their lives, and in 6-9% of them, chronic vulvovaginal candidiasis develops in the future, the cause of which in 90% of cases is Candida albicans.
The main factors in the development of candidal vaginitis are considered uncontrolled use of antibiotics, pregnancy, immune suppression and diabetes mellitus.
Methods for diagnosing vaginitis
Diagnosis of bacterial vaginosis includes: microscopic examination of secretions, bacteriological examination, determination of antigens of pathogens or determination of antibody titers by serological methods for the most common pathogens of vaginitis: facultative anaerobic microorganisms: Lactobacillus spp., Enterobacterium spp., Streptococcus spp .; obligate anaerobic microorganisms: Gardnerella vaginalis / Prevotella bivia / Porphyromonas spp., Eubacterium spp.; mycoplasmas: Mycoplasma hominis / Mycoplasma genitalium; mushrooms: Candida spp.
Basic principles of treatment of bacterial vaginosis
Systemic treatment for bacterial vaginosis includes:
1) metronidazole 400-500 mg orally twice a day for 5-7 days (first-line drug).
1) clindamycin (Dalacin) − 1 vaginal suppository for 7-10 days.
Restoration of normal vaginal biocenosis with preparations containing bifidobacteria and lactobacilli after antimycotic treatment:
- Vagilak − 1 vaginal suppository for 10 days.
During pregnancy (II and III trimester) and breastfeeding, only topical drugs are prescribed, it is also necessary to avoid the use of high doses.
For all types of vaginitis / vaginosis, topical antibiotics, in particular clindamycin, with the combined use of an antifungal drug, in particular miconazole, are advisable. At the same time, the use of topical drugs can significantly reduce the risk of systemic adverse reactions. It is important to note that the sexual partner also needs to be treated to avoid re-infection.
Vulvovaginal candidiasis: is fluconazole compatible with pregnancy






